Think you have sleep apnoea?
Sleep apnoea is when you stop breathing when you are asleep. Most commonly this is because something blocks your airway and is called obstructive sleep apnoea or OSA. When we sleep, our muscles relax, including our throats, that help keep our airway open.
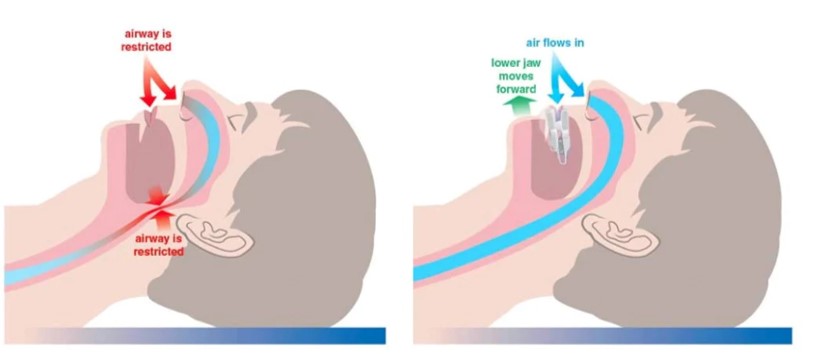
In OSA, these muscles can relax too much and block the airway, making it hard to breathe and result in you snoring! The causes of snoring and sleep apnoea are very similar and the overwhelming majority of sleep apnoea sufferers are heavy snorers.
Did you know?
Your brain is wired to look out for dangers, so when your oxygen level drops or carbon dioxide levels rise when you are asleep it wakes you up to start you breathing again. Often we go right back to sleep without knowing we woke up, however when we wake in the morning we are not refreshed. Without proper sleep your body can experience a build-up of toxins and inflammation.
When the oxygen saturation levels drop your body is in survival mode and releases stress hormones in response. Over time, this repetitive release of hormones will lead to high blood pressure and contribute to heart problems.
You are more likely to have OSA if:
Overweight or large neck circumference (over 16 inches if you’re a woman or 17 inches if you’re a man). 1
Certain medical conditions. E.g. Congestive heart failure, high blood pressure and type 2 diabetes
A family history of OSA
As we age, especially men as the elasticity of our tissues reduces
Smoke or drink (especially close to bedtime)
Problems of the mouth, nose, or throat that narrow the airway
A large tongue, which can fall back and block the airway during sleep
Symptoms
Daytime fatigue- due to lack of deep restorative sleep. Morning headaches, having trouble concentrating, irritable or depressed.
High blood pressure or heart problems.
Sudden drops in blood oxygen levels during OSA increase blood pressure and strain the cardiovascular system. In turn this leads to increased risk of stroke, heart attack, stroke and irregular heartbeats, such as atrial fibrillation.
Type 2 diabetes. Having untreated sleep apnoea alters glucose metabolism, promotes insulin resistance and thus increases your risk of developing type 2 diabetes.
How Is Obstructive Sleep Apnoea Treated?
When obstructive sleep apnoea is mild, it may be a matter of lifestyle change such as loosing weight, and sleeping on your side. Myofunctional therapy Yulli Tamayo-Myerson has been show to help to reposition the tongue, improve nasal breathing, and increase muscle tone protecting the airway.2
For anything more severe the gold standard treatment for obstructive sleep apnoea remains CPAP (continuous positive airway pressure). You wear a mask when you sleep (that covers the nose only or the nose and mouth) with a tube attached that pumps air into the airway and keeps it open. CPAP can be tough for many patients to wear, you end up with marks on your face in the morning and a dry mouth.
An alternative choice to CPAP is a custom mouth piece worn while sleeping.
These devices are called mandibular advancement appliances or splints. They work by holding the lower jaw forward and thereby keep your airway open during sleep. They can be made by a sleep apnoea trained dentist in as little as a week. I have made hundreds of these devices for my patients.
Nutrition
As we know the body craves fresh food. Especially living in UK sunlight is low and 1 in 6 adults and almost 20% of children in the UK are deficient in Vitamin D. Vitamin D regulates the amount of calcium and phosphate in the body. It is needed to keep bones, teeth and muscles healthy. Several studies suggest that in OSAS patients’ serum levels of vitamin D are lower compared with non-apnoeic subjects.
However, the mechanisms linking vitamin D deficiency and OSAS are not completely understood. When you have low vitamin D levels, it can make you fatigued, depressed, and cause a weakened immune system. I suggest all my OSA patients have their Vitamin D levels checked as it is simple to supplement. Also bear in mind that having low vitamin D levels is often caused by poor gut health, so checking your gut microbiome would also be prudent.
Snoring
Snoring at night is common however it is not normal. It does become worse as we age, due to the weakening neck muscles. It affects 30% of men and 20% of women under the age of 60, increasing to 60% and 40% over the age of 60.
Traditionally we were sent to hospital to be monitored overnight. I cannot think of a worse environment to try and get to sleep than a busy hospital ward wired up to multiple electrodes and being checked on with doctors in white coats.
Then classified as either mild, moderate or severe. This is set by the number of pauses in breathing per hour (AHI). Severe obstructive sleep apnea means that your AHI is greater than 30 (more than 30 episodes per hour).
Moderate with an AHI is between 15 and 30 and Mild your AHI is between 5 and 15
There is a better way! We have partnered with Itamar Medical Ltd that produces WatchPAT ONE a single use device that you wear overnight and it calculates AHI using your True Sleep Time and even measure the decibels of your snoring! It is a watch, finger probe and chest sensor.
For only £200 this will revolutionise the diagnoses of sleep apnoea.
Please speak to your dentist about sleep, we can help you feel refreshed again in the morning.
1. Neck circumference, metabolic syndrome and obstructive sleep apnea syndrome; Evaluation of possible linkage. Med Sci Monit. 2013 Süleyman Ahbab et al.
2. Orofacial Myofunctional Therapy in Obstructive Sleep Apnea Syndrome: A Pathophysiological Perspective. Medicina (Kaunas). 2021 Apr. Venkata Koka et al.
3. The role of vitamin D in obstructive sleep apnoea syndrome. Breathe (Sheff). 2018 Sep Kostas Archontogeorgis et al.

